SHOULDER
Proximal humerus fracture
Proximal humeral fractures are a common type of fracture, accounting for 4-6% of all fractures. It is the third most common type of non-vertebral fracture in the elderly, particularly those over 65. It is twice as common in women. Increasing age is associated with more complex fracture patterns
What is it?
Fractures of the proximal humerus can occur at a variety of sites, including the surgical neck, anatomical neck, greater tuberosity and lesser tuberosity, with surgical fractures of the two-part neck being the most common. There are several associated risk factors, including osteoporosis, diabetes, epilepsy and female gender.
Proximal humeral fractures: Etiology, symptoms and diagnosis
The etiology of these fractures can be attributed to a variety of factors. The mechanism of injury differs according to age group. In older people with osteoporotic bones, low-energy falls are the main cause. Conversely, high-energy trauma in younger individuals is more likely to result in humeral fractures, often accompanied by soft-tissue and neurovascular damage. Nerve damage, particularly to the axillary nerve, is a frequent complication associated with humeral fractures. Arterial lesions are rare, with an incidence of 5-6%, and more frequent in elderly patients. They often occur at the surgical neck or with subcoracoid dislocation of the head.
A fracture of the proximal humerus usually manifests itself as pain and swelling around the shoulder. There may also be decreased range of motion, particularly when attempting to abduct the arm. On physical examination, there may be extensive bruising of the chest, arm and forearm. A thorough neurovascular examination is important, as axillary nerve injury is the most common associated lesion. Deltoid muscle function and sensation over the lateral shoulder should be assessed. Arterial lesions may also occur, although these are rare, and may be masked by extensive collateral circulation preserving distal pulses. A concomitant chest wall lesion should also be sought during the examination.
Fractures of the proximal humerus are usually diagnosed with a combination of different imaging modalities. X-rays are the initial imaging modality of choice. CT may be indicated in certain cases where preoperative planning is required; if the position of the humeral head or major tubercle is uncertain, or if there is intra-articular comminution or risk of head fracture. MRI is rarely indicated, but can be useful in identifying associated rotator cuff lesions.
Conservative treatment
Conservative treatment is a reasonable approach for most fractures of the proximal humerus, involving a period of immobilization in a sling with limited, controlled amplitude and load, followed by progressive rehabilitation. This approach is indicated for most minimally displaced surgical and anatomical neck fractures, as well as for major tubercle fractures displaced by less than 5 mm. However, if the displacement is greater than 5 mm, impingement with loss of abduction and external rotation will result, necessitating surgical treatment. Age, fracture type, fracture displacement, bone quality, dominance, general health and associated injuries must be taken into account when choosing the optimal treatment. Immediate physiotherapy leads to faster recovery results.
Closed reduction with percutaneous pinning
Closed reduction with percutaneous pinning is a surgical technique used to treat certain types of fracture of the proximal humerus. This technique involves the placement of pins through the skin and into the bone to stabilize the fracture. It is most commonly used for two-part surgical neck fractures and certain valgus-impacted three-part and four-part fractures in patients with good bone quality, minimal metaphyseal comminution and an intact medial calcar. However, it has a considerably higher complication rate than other surgical techniques. The axillary nerve is at risk with lateral wires, while the musculocutaneous nerve, cephalic vein and biceps tendon are at risk with anterior wires. Consequently, the decision to use this technique must be taken with caution, taking into account individual patient factors such as age, fracture type, bone quality and general state of health.
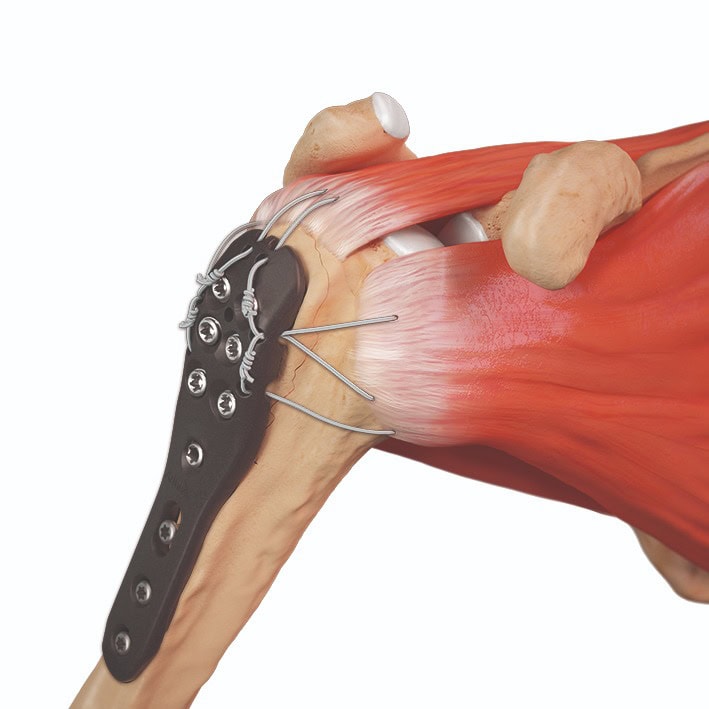
Open reducer with internal plate mounting
Arthrex GmbH 2024
Open reduction with internal plate fixation is indicated for fractures with a major tuberosity displaced by more than 5 mm, displaced 2-part fractures, 3- and 4-part fractures in young patients, and fractures with a split in the head. This technique has a lower complication rate and can be used for more complex fractures. It can provide excellent functional results, but is associated with a higher risk of avascular necrosis, particularly in displaced 4-part fractures.
Centromedullary nailing
Centromedullary nailing is indicated for surgical neck fractures or 3-part major tubercle fractures in younger patients, as well as combined fractures of the proximal humerus and humeral shaft. This technique offers favorable results in terms of fracture consolidation and range of motion, but is biomechanically inferior to plate fixation in terms of torsional stress. There is, however, an iatrogenic risk of fracture, particularly in osteoporotic bone.
Partial joint replacement: hemiarthroplasty
In cases where the articular surface of the shoulder is damaged, or where you have poor bone quality, partial joint replacement may be necessary. Hemiarthroplasty involves replacing the damaged or displaced humeral head with a prosthetic implant, while leaving the scapula cavity intact. It is recommended for younger patients (aged between 40 and 65) with complex fractures or head fractures that may fail fixation. Reverse total arthroplasty, on the other hand, is indicated for the undemanding elderly with non-reconstructible tuberosities and poor bone quality, or for elderly patients with fracture-luxation. This technique involves removing the damaged articular surface and replacing it with a prosthetic implant that has a ball-shaped end and a cavity-shaped end (in a healthy shoulder, the ball-shaped end of the humerus fits into the cavity of the scapula, in a reverse arthroplasty, the ball and cavity are reversed: the ball end of the implant is attached to the scapula and the cavity end is attached to the humeral bone). Results depend on tuberosity reduction and consolidation, restoration of humeral height and version. Poor results can occur with pseudarthrosis or callus of the tuberosities and humeral retroversion of more than 40°.
Possible complications and post-surgery exercises
There are specific and general complications associated with these surgical techniques. The most frequent complication of plate fixation is screw detachment, with an incidence of up to 14%. Avascular necrosis of the humeral head is another complication, but is better tolerated than in the lower limbs. Nerve damage can occur, with axillary nerve damage the most common, with an incidence of up to 58%. Malunion and non-union (pseudarthrosis) are also possible; if the patient is elderly, this is an indication for a total reverse prosthesis; smoking and age are risk factors. Other potential complications include damage to the rotator cuff and long biceps tendon, undiagnosed posterior dislocation, retractile capsulitis and scar tissue, post-traumatic arthritis and infection. Consequently, careful consideration of the risks and benefits of each treatment option and meticulous surgical technique are essential to minimize the risk of complications.
After surgery, you’ll usually need a period of immobilization in a sling or corset for several weeks to allow the bone to heal. Rehabilitation exercises are usually started soon after surgery to help restore shoulder range of motion and strength. These exercises can include gentle stretching, resistance exercises and activities to improve coordination and balance.