SHOULDER
Shoulder dislocation
Shoulder dislocation is one of the most common shoulder injuries, with an annual rate of 1.7% in the general population. Patients in the military and those involved in contact sports are at increased risk of shoulder dislocation.
Incidence of recurrence
The incidence of recurrence is high, and correlates with the age at which the initial dislocation occurred. Adolescents have a significantly higher rate of recurrence, with up to 80-90% of them suffering another dislocation. Patients under 20 have a 90% chance of recurrence.
Risk factors

Arthrex GmbH 2024
It can be caused by a variety of factors, including trauma, congenital laxity and repetitive overhead movements. This results in damage to the soft tissues and bony structures of the shoulder joint. A characteristic lesion of this condition, present in 80-100% of cases, is the Hill-Sachs lesion (posterolateral cortical depression of the head of the humerus). This can have important implications for surgical management, with the concept of “on-track” versus “off-track”, the aim being to convert an “off-track” lesion into an “on-track” lesion.
Shoulder instability can be associated with multiple orthopedic and medical pathologies. Orthopedic pathologies include labrum and cartilage lesions such as Bankart’s lesion (avulsion of the anterior labrum and the anterior band of the inferior glenohumeral ligament from the anteroinferior glenoid), present in 80 to 90% of cases; humeral avulsion of the glenohumeral ligament, with a higher recurrence rate; glenolabral lesion (lesion of the anteroinferior labrum), a risk factor for failure after arthroscopic stabilization procedures; and ALPSA (anterior labral periosteal sleeve avulsion), also a risk factor for failure. Associated bone lesions include Bankart’s bone lesion (fracture of the anteroinferior glenoid), present in 49% of patients with recurrent dislocations, it should be addressed as it implies an increased risk of failure of arthroscopic treatment; the previously mentioned Hill-Sachs lesion, which usually has no clinical implication; fracture of the greater tuberosity, associated with a higher risk of recurrence; fracture of the lesser tuberosity, associated with posterior dislocations. Nerve lesions, such as axillary nerve damage and rotator cuff tears, are also associated with shoulder instability. Patients with overall ligament hyperlaxity (Ehlers-Danlos syndrome, collagen pathologies…) are at increased risk of developing shoulder instability, which in this case is more often recurrent and atraumatic. It is important to identify these associated lesions, as they may require additional surgery and affect the management of the primary instability.
Examination and assessment of shoulder instability
When a patient presents with possible shoulder instability, it’s important to obtain a thorough history and physical examination. Patients often recall a traumatic event leading to dislocation, and may have undergone forced or spontaneous reduction. Symptoms include a feeling of instability and shoulder pain due to subluxation or impingement of the humeral head on the glenoid. The physical examination includes several tests, including the “load and shift” test, which assesses the amount of glenohumeral translation, the apprehension sign, which is positive when the patient feels apprehension, and the recentering sign, positive when it shows a decrease in apprehension with anterior force applied to the shoulder. Ligament laxity can be assessed according to the Beighton criteria or specific shoulder laxity criteria.
Imaging plays an important role in the assessment of shoulder instability. X-rays are the imaging modality of first choice, providing a good overview of the shoulder joint. MRI is the preferred imaging modality for visualizing labral tears. MRI arthrography has a higher sensitivity and specificity for detecting soft tissue lesions than conventional MRI. Bone status of the glenoid and humerus is better defined with 3D CT reconstruction.
Treatments for shoulder instability

Arthrex GmbH 2024
Treatment of shoulder instability may be conservative or surgical, depending on the severity of the dislocation and other factors. Following reduction of the dislocation, conservative treatment involves a period of immobilization of at least one week with limited and controlled amplitude and load, followed by a period of physiotherapy with the aim of strengthening the shoulder’s dynamic stabilizers such as the rotator cuff and periscapular musculature. Risk factors for reluxation include age under 20, male gender, contact sports, hyperlaxity, glenoid bone loss of more than 20-25% and major tubercle fractures.
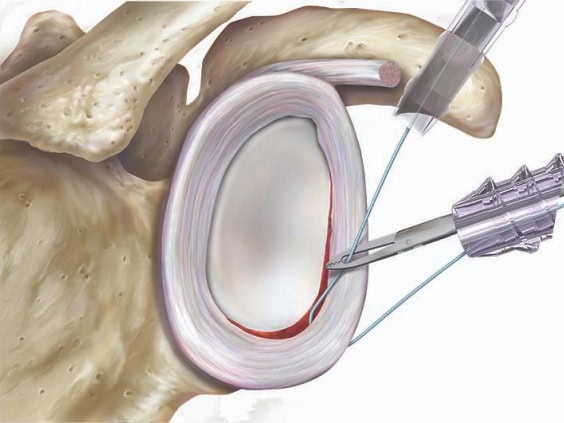
Arthroscopic Bankart repair
Surgical treatment involves arthroscopic Bankart repair. Indications for surgery include a first traumatic shoulder dislocation with an MRI-confirmed Bankart lesion in athletes under 25 years of age, requesting athletes, recurrent dislocation/subluxation following conservative management, and glenoid bone loss of less than 20-25%. The results of arthroscopic repair are now as effective as open repair, with the advantage of less pain and greater preservation of motion. Higher failure rates are observed in patients with overall hyperlaxity or glenoid bone loss.
Latarjet procedure
The Latarjet procedure is indicated in cases of glenoid bone loss greater than 20-25% or an “off-track” lesion. This technique involves transferring the coracoid bone with the attached conjoint tendon and coracoacromial ligament. The rate of recurrent instability varies from 0% to 8%, and good results are observed in over 90% of patients.
Autograft and allograft bone transfer
Autograft and allograft bone transfer procedures are indicated for patients with greater than 20-25% glenoid bone deficiency in whom the Latarjet procedure has failed. An iliac crest or distal clavicle autograft or an iliac crest or distal tibia allograft can be used in these procedures. The technique can be performed arthroscopically or openly. The results of these procedures are generally good, with a healing rate of 89% at an average of 1.4 years.
When the patient has large Hill-Sachs lesions (25-40% of the humeral head) or “off-track” lesions, filling of the lesion can be combined with Bankart repair (open or arthroscopic). By reducing the size of this lesion, the procedure converts an “off-track” lesion into an “on-track” one. The results of this procedure are promising. The Latarjet procedure remains an alternative with comparable results. When the Hill-Sachs lesion is particularly large, generally exceeding 40% of the humeral head, bone graft reconstruction is indicated. The technique involves using an allograft to fill the defect in the humeral head, with the aim of improving stability and reducing the risk of recurrent dislocation. Arthroplasty and rotational osteotomy may also be options in cases where damage is particularly severe.
Tendon transfers
Tendon transfers can be used to treat a chronic, irreparable subscapular tear. One option is to use the latissimus dorsi muscle as a tendon transfer, which can better reproduce the line of traction of the native subscapularis muscle. Another option is to use the pectoralis major muscle, in particular the sternal head.
Possible complications
Recovery and rehabilitation protocols vary according to the specific procedure performed, but generally include a period of immobilization with limited and controlled amplitude and load, followed by a gradual return to activity with the help of physiotherapy. Complications can be divided into early and late complications. Recurrence of instability is a common early complication, and may be due to unrecognized glenoid bone loss, poor surgical technique or preoperative risk factors such as age, gender and sporting activity. Shoulder pain can occur if the labrum repair is too tight, leading to arthropathy. Nerve damage is another potential early complication, with the musculocutaneous nerve most often affected. Stiffness, particularly in rotation, may occur after Latarjet surgery or filling. Infections, material complications such as anchor (in Bankart repair) or screw (in the Latarjet procedure) removal, or graft lysis (in the Latarjet procedure) are other early complications that can occur.